Abstract
Background
Bariatric surgery results in changes in mental health, quality of life and social functioning, but these results differ among individuals. In this study, we examine the psychosocial experiences of patients following bariatric surgery and clarify the factors at an individual level that can change psychosocial outcomes.
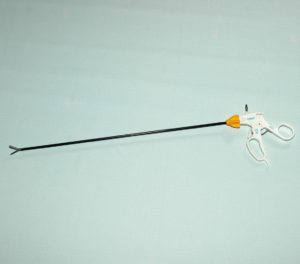
Click here: Bariatric Surgery Instruments
Methods
Eleven semi-structured focus groups with Bariatric Surgical Cooperative patients (n = 77). Interviews were recorded, word-by-word transcribed, and analyzed using an established theory approach. Data on participants’ demographic characteristics was extracted from the clinical program.
Results
The majority of the focus group participants were women (89%), white (64%), and married (65%). We identified three main themes: (1) change in self-perception; (2) change others; and (3) change relationships. Each theme comprises 3 sub-themes, reflecting a range of positive and negative psychosocial experiences. For example, weight loss resulted in increased self-confidence among many participants and others attributed loss of identity. Some noted that they had a better relationship with family or friends.
Conclusion
Weight loss following bariatric surgery results in complex changes in self-evaluation and interpersonal relationships, which may be a pro-active mediator of commonly assessed mental health outcomes such as depression. Individuals considering bariatric surgery may benefit from projected guidance on these different experiences, and long-term surgical monitoring should include evaluation of adverse psychosocial events.
Background
The burden of obesity health cannot be denied. Within the, more than a third of adults live with obesity and more than six hundred million adults worldwide – obesity lasts at 11% of men and 15% of women.. Moreover, an increasing number of people are living with morbid or severe obesity (body mass index> 40 kg / m2), which has serious health consequences and contributes significantly to obesity-related healthcare expenditure. The bariatric surgery, including gastric bypass, sleeve gastrectomy, and laparoscopic gastric banding, is the most effective treatment for morbid obesity, and often reduces the extra weight within one year of surgery. for a long period. Apparently after post-surgical weight loss, control of chronic conditions associated with obesity such as diabetes type 2 mellitus is solved and / or improved.
As well as poor physical health, people with obesity are more likely to experience mental ill-health and factors such as stigma associated with weight, discrimination, and poor body image have a social dysfunction. Psychosocial changes occur after severe weight loss after bariatric surgery. However, in contrast to the predictable mental benefits of major weight loss, there are different psychosocial outcomes among patients and there is little information on the experiences at an individual level that could contribute to these variations. For example, many people have reduced depression and increased standard of living after bariatric surgery. But others can only get a psychological benefit in the short term or not at all.
Post-surgical weight loss can be affected by poor mental health, and psychosocial performance is commonly considered before bariatric surgery using standardized tools and clinical interviews. However, there are no definitive guidelines for this process and the accuracy of these assessments may be undermined by the under-reporting of patients to psychological dysfunction. Following bariatric surgery, psychosocial performance is not routinely assessed in the clinical setting. Among researchers, quantitative psychometric tools are usually used to assess post-surgical depression intensity and health-related living standards (eg Weight Impact on Quality of Life, Survey Form Short ). While these instruments can clarify general trends and associations, they fail to capture the experiences of surviving at an individual level that may drive change in outcomes (eg increased marriage discord after major weight loss). The hypothesis mechanisms for improved mental health include increased self-confidence, improved self-image, and improved relationships as a result of major weight loss. On the other hand, mental health may be exacerbated by unrealistic pre-surgical expectations about the potential physical and mental benefits of weight loss or unforeseen changes in social relationships.
In this study, we carried out semi-structured focus groups with 77 US adults who had bariatric surgery, and we attribute patient-level experiences that could push differences in psychosocial outcomes after severe weight loss. This data could facilitate more personalized counseling before bariatric surgery, and may give patients a broader understanding of the psychosocial risks and benefits that bariatric surgery may have in the context of their individual lives. Moreover, this data may inform post-operative strategies for discussing psychological malfunction, identifying and treating after weight loss surgery.
For more information visit our website Bariatric Surgery Instruments



